At the completion of this article, the optometrist should be able to understand their role in management of patients with keratoconus, including:
- Understand the crucial role optometrists play in identifying candidates for CXL
- Understand how imaging modalities have improved a clinician’s diagnostic ability for early stages of keratoconus
- Be able to provide patient education on CXL protocols and post-operative recovery.
Dr Judy Y.F. Ku
MBChB, FRANZCO
Honorary Clinical Associate Professor, Faculty of Health,
School of Optometry and Vision Science, QUT
Cataract, Anterior Segment and Glaucoma Surgeon,
OKKO Eye Specialist Centre
While ophthalmologists play a critical role in managing moderate to advanced stages of keratoconus, Dr JUDY KU delves into the vital role that optometrists have in early diagnosis and treatment, ultimately contributing to better patient outcomes.
Defining keratoconus
Keratoconus (KC) is a bilateral asymmetric, ectatic corneal condition that is characterised by progressive thinning and steepening of the cornea, causing irregular astigmatism and visual disturbances.
Typically, it develops during adolescence or early adulthood; children are more likely to have severe disease at the time of diagnosis (27.8%) and progress more rapidly (88%).1,2
Conservative treatments such as spectacles and contact lenses (CL) may not be sufficient as the disease progresses and, in advanced cases, corneal transplantation may be necessary. With the advent of corneal collagen cross-linking (CXL) which halts progression, the rates of corneal transplantation have reduced substantially.3
This is why early diagnosis and prompt treatment of keratoconus is essential in preventing progression and mitigating its impact on patients’ quality-of-life.
Epidemiology and risk factors
The prevalence of keratoconus has been estimated at 1:375 to 1:2000 people. A much higher rate has been reported among certain ethnic groups, in particular Asian, Middle Eastern, Maori and Polynesians.4 A recent Australian study, based on a predominantly Caucasian young adult population, has shown an even higher prevalence (one in 84) than previously reports.5 In turn, this has important public health implications and due to this, early screening and treatment is recommended to improve quality-of-life and reduce social and financial burden.
The etiology of keratoconus is not fully understood, but it is thought to be an interplay between genetic predisposition and environmental factors, as well as biomechanical factors such as eye rubbing and ocular compression. Atopic disorders are well documented risk factors, such as allergic keratoconjunctivitis, eczema and atopic dermatitis which often leads to chronic eye rubbing. Contact lens wear is also an association and thought to be linked to microtrauma.
There is growing evidence that a history of asthma is associated with an increase in the severity of keratoconus.6 Other risk factors include a positive family history, Down’s syndrome, floppy eyelid syndrome and connective tissue diseases (Marfan’s syndrome).
Optometrists need to be aware of these risk factors which may trigger further investigations to identify early keratoconus.
The importance of early diagnosis
As keratoconus tends to affect young adults in their prime, it has a significant impact on a patient’s quality-of-life. In addition, paediatric keratoconus (onset before 18 years of age) tends to be more advanced and progress more rapidly than adult keratoconus.1,2
There has been a paradigm shift in the management of keratoconus, with a particular focus on early intervention to maintain vision and corneal integrity.
Corneal collagen cross-linking is a highly innovative and minimally invasive technique that has been proven to slow progression and reduce the rates of corneal transplantation. As a consequence, identification of those suitable for CXL at early stages would ensure that they are amenable to less-invasive treatments and maintain their functional vision in spectacles and contact lenses for as long as possible.
In addition, keratoconus patients usually develop myopia and astigmatism and may seek corneal refractive surgery/laser vision correction. Screening for subclinical asymptomatic keratoconus is critical in avoiding refractive surgery-induced corneal ectasia in this population.
Nomenclature for mildest form of keratoconus
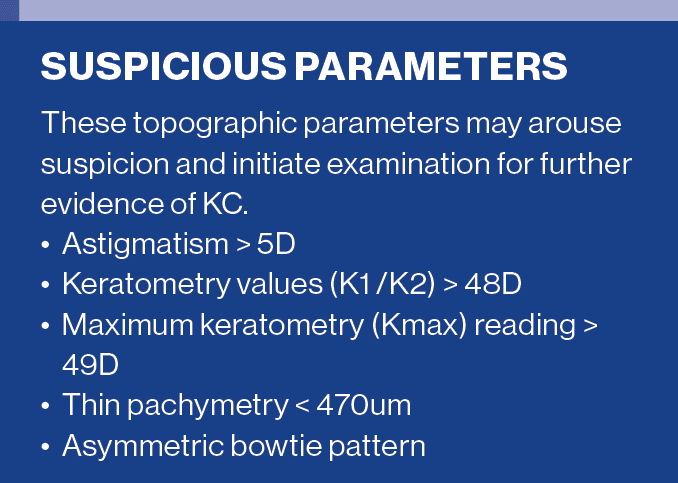
Various terms have been used interchangeably to describe the mildest form of keratoconus. To avoid confusion, it has been proposed to further define these terms:7
1) Forme fruste keratoconus (FFKC) – contralateral eye of KC patients with no clinical signs or topographic abnormalities
2) Keratoconus suspects, preclinical or subclinical KC – corneas with no slit lamp signs but inferior corneal steepening/asymmetry on topography with unaffected visual acuity
Clinical diagnosis of mild keratoconus relies on imaging
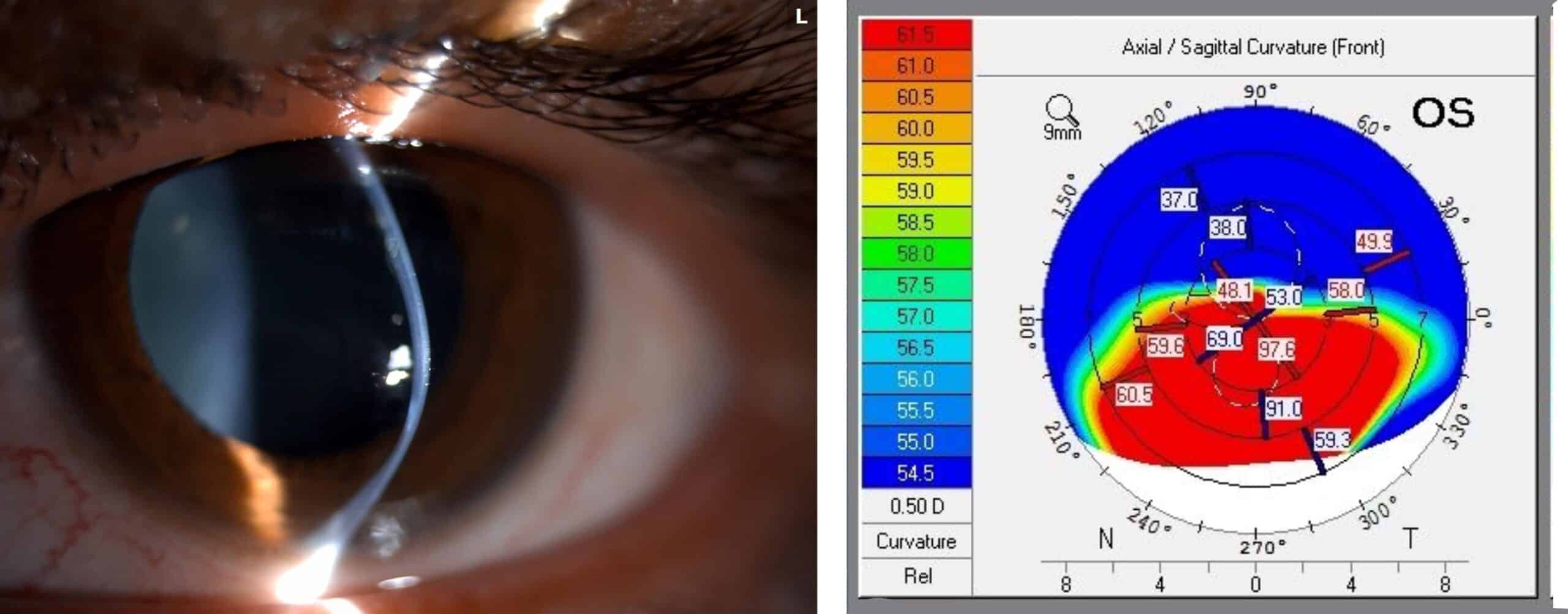
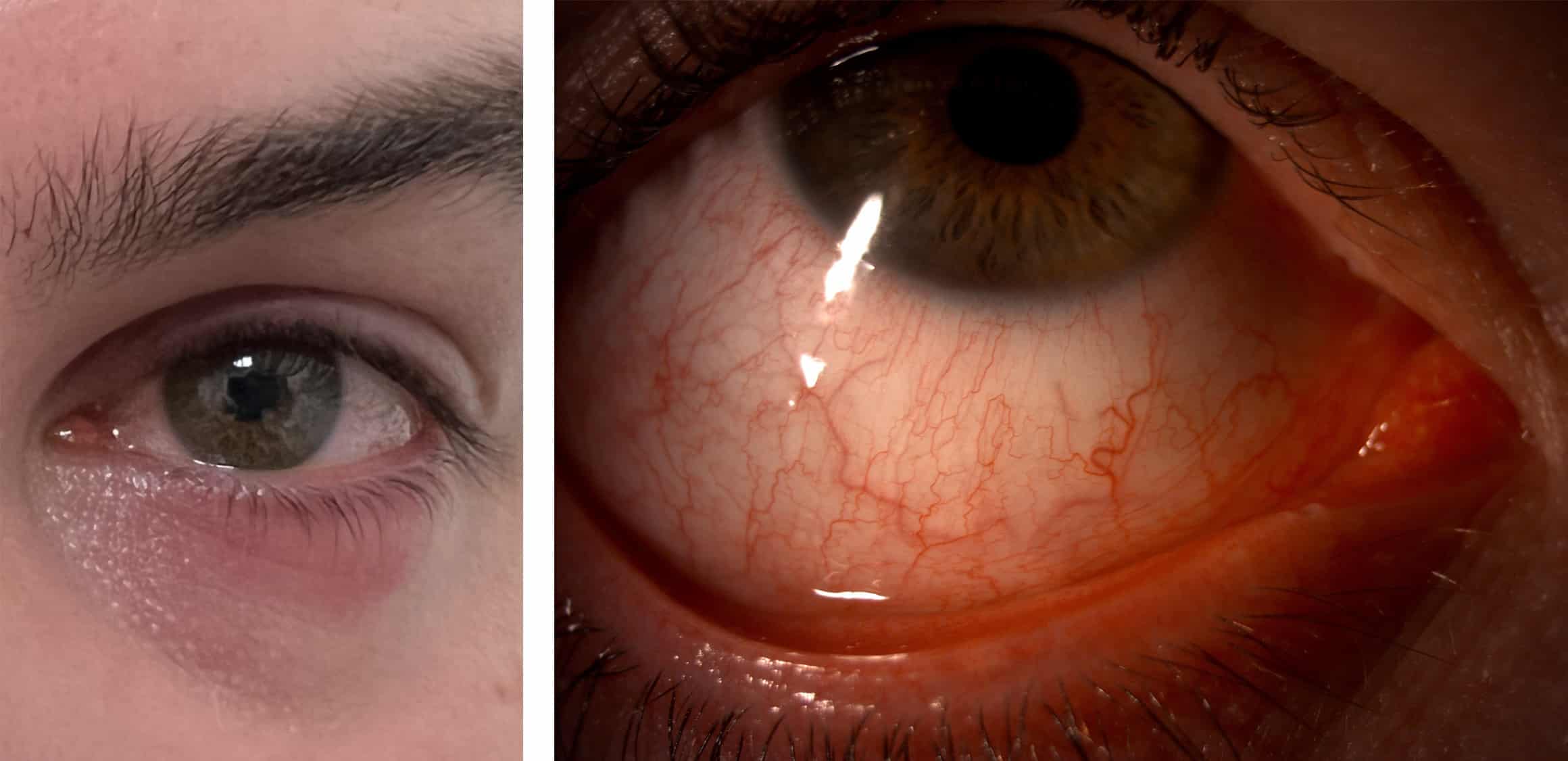
Identification of milder forms can be challenging as the majority of cases are asymptomatic with no obvious clinical signs (Figures 1A and 1B). It requires the optometrist/ophthalmologist to have a high index of suspicion, especially in patients with risk factors.
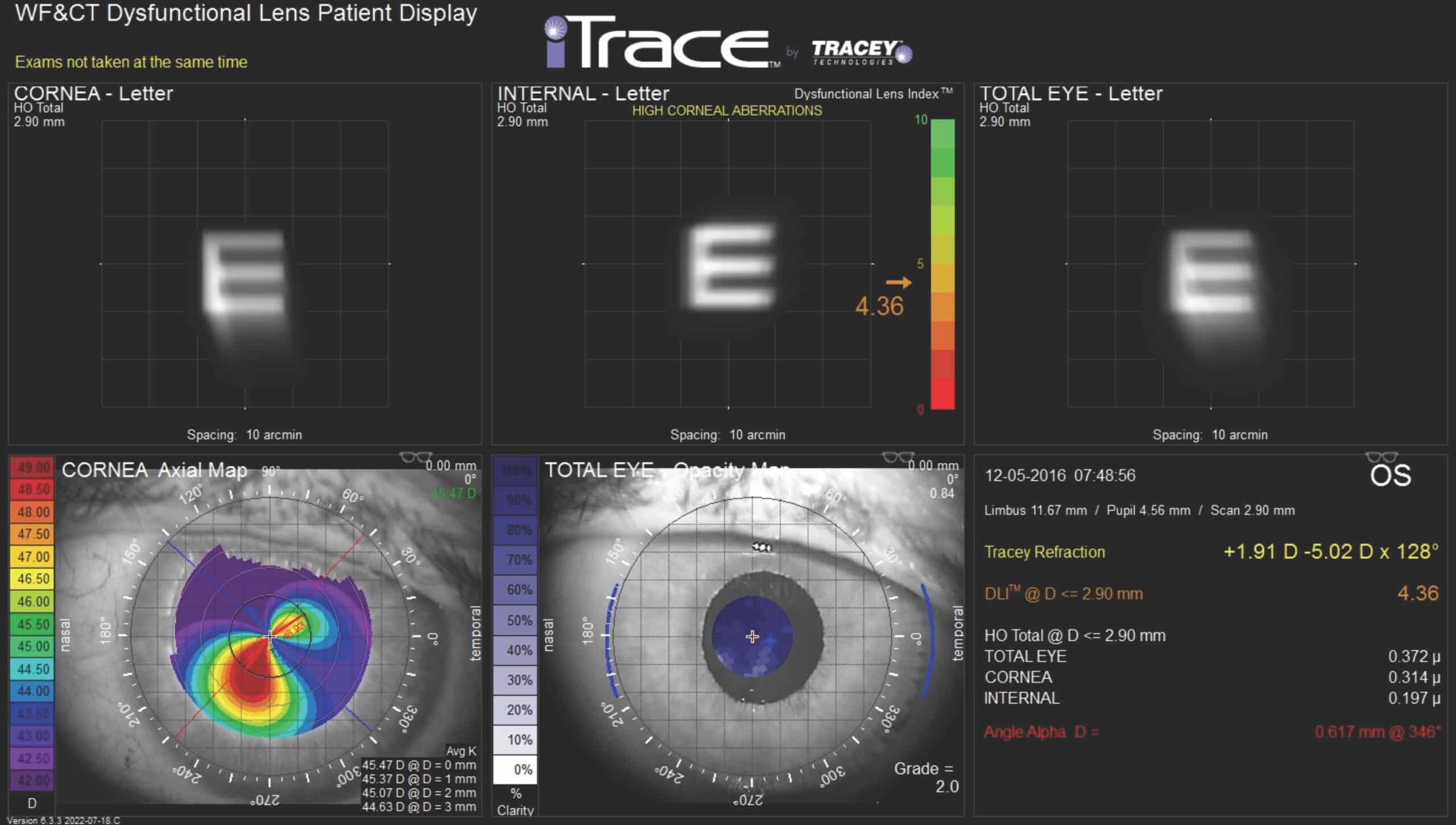
The availability of various imaging modalities has improved a clinician’s diagnostic ability for early stages of keratoconus. Placido disc-based topographers are now commonly available in optometry practices which can reveal clues such as irregular astigmatism and localised corneal steepening. However, these are based only on the anterior corneal surface and thus tear film instabilities can have a significant impact on its accuracy.
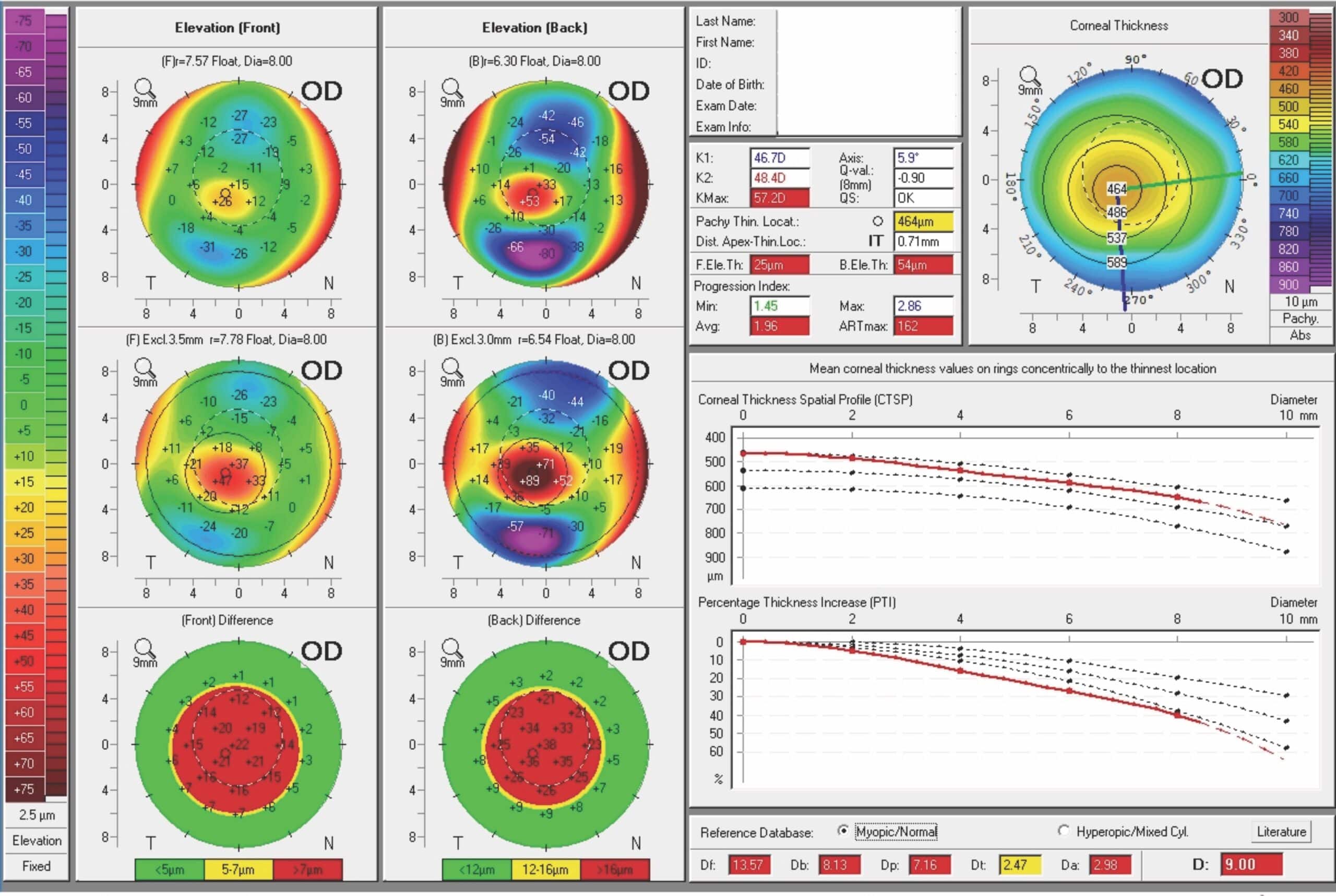
Corneal tomography (for example, Pentacam) on the other hand is a 3D imaging system which measures both the anterior and posterior corneal surface along with a full pachymetric map. Abnormal posterior corneal changes and/or pachymetric changes are typically the first indicators of subclinical keratoconus despite normal anterior curvature. Therefore if there is clinical suspicion, but the initial topography is normal, the optometrist should refer the patient to their local ophthalmologist for further specialised testing.
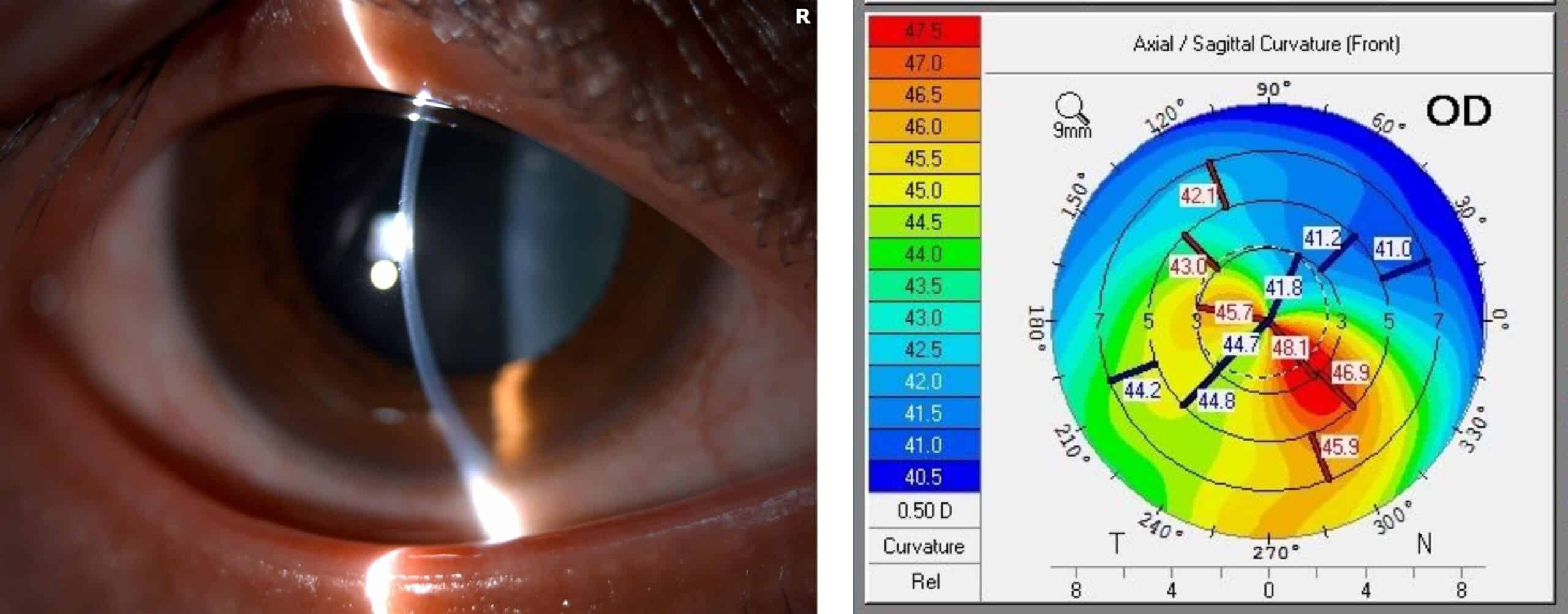
Clinical presentation of moderate to severe keratoconus
Optometrists, being primary eyecare providers, are well-positioned to detect clinical findings suggestive of keratoconus during routine exams. In moderate to advanced keratoconus, significant visual distortion may be reported – for example, ghosting and halos, sensitivity to glare and flaring of vision at night time and blurry vision (Figure 2).
Patients may present with frequent changes in glasses prescriptions and a progressive increase in astigmatism. Classic signs such as scissoring reflex or the Charleaux/oil droplet sign on retinoscopy are further diagnostic clues. Other slit lamp findings include stromal thinning/scarring, conical protrusion, Fleischer’s ring, Vogt’s striae, thickened corneal nerves and Munson’s signs.
Case report: Dual pathologies
Be mindful that patients can have co-existing diseases. Case A is a 32-year-old man with a history of juvenile open angle glaucoma who has been on glaucoma medications since the age of 10. This caused intermittent ocular surface inflammation and irritation (Figures 3A and 3B). When he was referred for ongoing glaucoma care, we noted much higher astigmatism and reduced BCVA in the right eye (6/21 unaided 6/9 with +0.25/-2.75 x 55) compared to his left eye (6/18 unaided 6/6 with -1.50/-0.25x 10). His pachymetry was also asymmetric (RE 487um LE 528um).
Upon further questioning, he admitted to being a frequent eye rubber as he became sensitive to the glaucoma drops. He also reported a gradual deterioration of his right vision over the past nine years and a family history of keratoconus involving his brother. Pentacam tomography confirmed moderate keratoconus in the right eye and subclinical keratoconus in the left eye (Figures 4A and 4B). He subsequently underwent CXL in the right eye and had selective laser trabeculoplasty (SLT) to reduce his dependency on glaucoma drops. This case illustrated the fact that as clinicians, we must remain vigilant and when there are suspicious features (e.g. asymmetric astigmatism and thin central corneal thicknesses), even in the presence of co-existing disease, one should still investigate further to exclude keratoconus.

Early treatment of keratoconus
The most important goals of non-surgical management are to increase corneal stability and provide visual rehabilitation. From the outset, it is important to verbally educate the patients and carers about the importance of avoiding eye rubbing. Any associated atopy should be managed with the assistance of other disciplines such as general practitioners and dermatologists.
Some patients may require systemic antihistamines/steroid sparing anti-inflammatories if their eczema/atopic dermatitis is severe. Any ocular allergies or dry eyes should be treated with regular mast-cell stabiliser/antihistamine drops and lubricants.
Glaucoma drops related ocular allergies should be co-managed with their ophthalmologist to consider alternative treatment such as SLT or minimally invasive glaucoma surgery (MIGS). In terms of optical correction, optometrists typically provide a step-wise approach – that is, start with spectacles, soft contact lenses, rigid lenses then specialised CL such as hybrid, piggy-back, scleral and mini-scleral.
Corneal collagen cross-linking
Although optical correction assists with visual rehabilitation, only CXL can halt progression. The original Dresden protocol involves epithelial debridement, soaking the cornea with riboflavin drops for 30 minutes, followed by exposure to ultraviolet light for 30 minutes, thereby strengthening the collagen fibres.
Optometrists play a crucial role in identifying suitable candidates for CXL and referring patients in a timely fashion. It is prudent to provide any past refractive/topographic history to demonstrate progression which is required by Medicare.
As keratoconus progresses asymmetrically, paediatric patients often present late as they tend to maintain good binocular visual function until both eyes are affected. In addition, their corneal instability could progress in months rather than years. Hence all paediatric patients should be referred early to consider CXL due to its progressive nature rather than wait until signs of visual degradation have been detected.

The prognosis of corneal transplantation for paediatric patients is also much worse than adults due to an increased risk of rejection. Moreover, they need to be followed up long-term by their optometrists even after CXL as the regression rate is 24% in patients aged 15 years or younger.8 If CXL is being deferred in patients less than 15 years of age, then topography should be repeated every three months to closely monitor for progression.
On the other hand, adult keratoconus patients should be separated into two categories:
a) Progressive KC
Regardless of age, adults with symptoms or signs of progression or a number of risk factors, should be referred early to consider CXL or potentially other surgical correction if indicated.
b) Non-progressive KC
Keratoconus generally stablises in the third or fourth decade of life and some of these adults have managed well with optical correction with no progression for years. These patients do not need CXL but should instead be monitored by their optometrists. On the other hand, if they become CL intolerant, they should be referred for alternative management.
Contraindications for CXL include:
- Very thin CCT (<400um)
- Previous herpetic infection as it may result in viral reactivation
- Severe corneal scarring
- Reduced wound healing e.g. Neurotrophic keratopathy
- Severe ocular surface disease
- Pregnancy and breast feeding
These patients need to be educated about the importance of monitoring, greater risk of progression and possible surgical intervention in the future.
Post-operative care
After CXL, all patients require antibiotics and topical steroids. Acute pain management in the first 24-48 hours is crucial, which include a bandage contact lens, eye patch, cycloplegic drops (in paediatric groups) and regular systemic analgesics. It generally takes four days for epithelialisation to occur.
Regular preservative-free lubricants encourage faster healing. It is not uncommon to develop a mild stromal haze which decreases with topical steroids by two months postop. Over the ensuing months to years, there would be gradual central flattening and some may notice a mild improvement in vision.
After initial recovery, optometrists have an essential role in visual rehabilitation by managing patient’s contact lenses/spectacles and to monitor for progression. It is also an opportunity to ensure that their ocular allergies continue to be managed.
Other treatments
There are several adaptations of the original CXL protocol, with the goals of avoiding the need for epithelium debridement (transepithelial CXL), thereby reducing pain and the risk of infection, and reducing treatment time (accelerated CXL). However, the interest in transepithelial CXL is diminishing due to its inferior efficacy compared to epi-off CXL. Accelerated CXL is gaining popularity which reduces the UV time down to eight to 10 minutes, yet achieving similar efficacy to the standard protocol.
Intrastromal corneal ring segments (ICRS) is based on the principle that adding synthetic segments in the corneal periphery induces central flattening. This is a useful intermediary option for patients intolerant of CL and delay the need for keratoplasty.
Corneal allogenic intrastromal ring segments (CAIRS) is a new promising technique which utilises donor corneas. This improves biointegration with the host cornea, thereby reducing the risk of extrusion, infection and inflammation.
Corneal transplant is reserved for severe keratoconus not amenable to other treatments. Apart from penetrating keratoplasty, partial thickness transplants such as deep anterior lamellar keratoplasty (DALK) was developed to reduce the risk of graft rejection. Recently Bowman’s layer transplantation has been proposed to treat advanced KC and delay the need for DALK or PK. Further details of these procedures are beyond the scope of this article. After any corneal transplantation, optometrists play an important collaborative role in managing residual astigmatism and monitoring.
Summary
The early diagnosis and treatment of keratoconus relies on the expertise of both optometrists and ophthalmologists working in tandem. Optometrists, being primary eyecare practitioners, play a crucial role in detecting early keratoconus through thorough history taking (identifying key risk factors), comprehensive eye examination and imaging. Their collaboration with ophthalmologists ensures timely referral, accurate diagnosis, and the implementation of the most appropriate treatment strategies.
By working together, optometrists and ophthalmologists can effectively manage keratoconus thereby improving patients’ quality-of-life, and preventing further visual deterioration.
More reading
Collaborative care in keratoconus – Dr Brendan Cronin
Striving for new highs in keratoconus treatment
A new school in corneal collagen cross-linking
References
1.Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012;28(11):753–758.
2. McAnena L, Doyle F, O’Keefe M. Cross-linking in children with keratoconus: a systematic review and meta-analysis. Acta Ophthalmol. 2017;95(3):229–239.
3. Chan C. Corneal cross-linking for keratoconus: current knowledge and practice and future trends. Asia Pac J Ophthalmol. 2020;9:557-564.
4. Sahebjada S, Chan E, Sutton G, Pang CP et al. Keratoconus International Consortium (KIC) – advancing keratoconus research. BMC Ophthalmol 2023;23:337.
5. Chan E, Chong EW, Lingham G, Stevenson LJ, Sanfilippo PG, Hewitt AW et al. Prevalence of keratoconus based on Scheimpflug imaging: the Raine Study. Ophthalmology 2021;128(4):515-521.
6. Sahebjada S, Chan E, Xie J, Snibson GR, Daniell M, Baird PN. Risk factors and association with severity of keratoconus: the Australian study of Keratoconus. Int Ophthalmol. 2021;41:891-899.
7. Santodomingo-Rubido J, Carracedo G, Suzaki A, Villa-Collar C, Vincent SJ, Wolffsohn JS. Keratoconus: an updated review.Contact lens anterior eye. 2022;45(3):101559
8. Mazzotta C, Traversi C, Baiocchi S, et al. Corneal collagen cross-linking with riboflavin and ultraviolet A light for pediatric keratoconus: ten-year results. Cornea 2018;37(5):560-566.